Is a COVID-19 Vaccine Policy Right for Your Business?
Epistemix teamed up with Health Preparedness Partners to complete a prospective, scenario-driven study quantifying the impact of different vaccine policies on the return to the office across ten major American cities.
The results show how managers can increase productivity, decrease healthcare costs, and mitigate the risks associated with bringing employees back.
Major Takeaways
- Establishing a vaccination policy as part of return to office planning is an important part of protecting the workforce and the business.
In every city included in the study, companies with no return to office vaccination policy had higher employee absences and higher health costs compared with businesses that implemented any vaccination policy. - Businesses that required employees to be fully vaccinated before they returned to the office experienced no staff illnesses, missed workdays or increased expenses related to COVID-19.
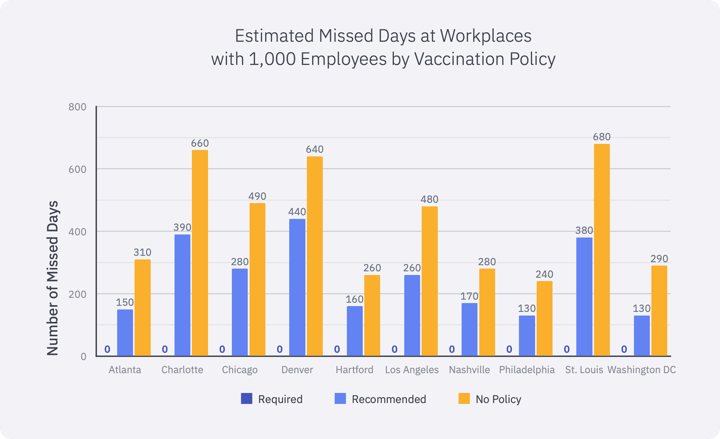
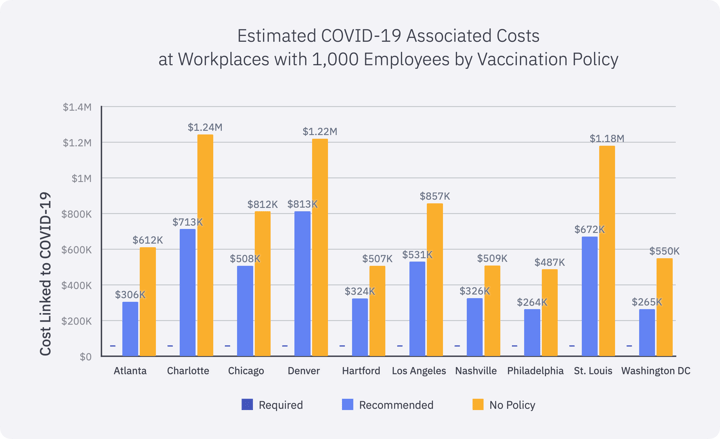
- Businesses of 1,000 employees without an employee vaccination policy are likely to have an estimated 392 missed days of work over the upcoming fall and may spend $798,000 on COVID-19 health costs, on average.
- Businesses can prevent nearly 200 missed workdays in the fall from employee absences and save around $326,000 by strongly encouraging employees to get vaccinated before returning to the workplace.
- Businesses that strongly encouraged vaccination before entering the workplace can reduce workplace absences due to illness and lower COVID-19 health costs by 59%, compared with having no vaccination policy.
- Businesses in cities with lower vaccination rates in working adults, such as Charlotte, NC would most benefit from a vaccination policy, preventing nearly 610 missed days in the fall and saving approximately $1.2M in COVID-19-related health costs.
- Businesses located in cities with higher levels of vaccination coverage in working adults, like Hartford, CT, could also realize savings from a vaccination policy of about $324,000 in COVID-19 related health costs and prevent up to 210 missed days over the fall.
In spring of 2020, the pandemic shut down offices across the country and fundamentally changed the way we work together. Organizations had no choice but to adapt. Now that COVID-19 disease levels are declining overall, stay-at-home orders have been lifted, vaccination levels are increasing, and employee working preferences have shifted, organizations need to adapt again.
Decisions must be made about when to return to the office and what policies should be implemented to protect the workforce and the business. Crafting a return to office plan that maximizes productivity and ensures employee health is an unprecedented challenge, but businesses have more control than they realize.
Over the course of the pandemic, operations, human resources, and enterprise risk managers lacked a common playbook to guide decisions. Most organizations sought out best practices by sifting through information from the World Health Organization, Centers for Disease Control and Prevention, their local health authorities, and, occasionally, consulting epidemiologists.
To decide when employees can safely return to the office, organizations must consider a variety of evolving factors: local policies, the level of pandemic spread in the community, employee willingness to return, business realities, status of workplace physical adaptations, and issues related to the commute and other community factors.1
Once a decision about when to return is made, the next problem is how to execute the return, particularly the company’s vaccination policy. Company vaccination policies should harmonize with the culture of the company. Two key metrics should guide decisions about how to execute the return: vaccination coverage in the cities where offices are located and employee vaccination rates. Using those two metrics as guideposts, organizations can use science-backed strategies to safely bring employees back to the office and address the challenges of managing productivity, health costs, and risks to business continuity.
Vaccines are a proven solution to reduce the number of COVID-19 cases and hospitalizations2 so organizations can safely have employees return to the workplace. Workplace policies should depend on whether employees are or are not fully vaccinated before they return to the office.
Health Preparedness Partners, a consulting firm that helps organizations in their response to the COVID-19 pandemic, worked with Epistemix to quantify the impact of different vaccine policies upon the return to the office. Insights from the study can empower leaders to manage risks that are within their control.
The study simulated the impact of various employee vaccination policies on productivity and health costs in ten cities within the United States where the percentage of adults that are fully vaccinated as of the first week in July ranged from 39% in Atlanta, Georgia to 71% in Hartford, Connecticut. The selected cities represent different geographies, individual behaviors, demographics, and vaccination coverage to show regional differences across the country. In each of the cities, a hypothetical workplace of 1,000 employees was simulated and three workplace vaccination policies3 were tested:
- All employees are asked to be vaccinated before returning to office;
- Getting vaccinated before returning to the workplace is strongly encouraged, but not required;
- No vaccination policy.
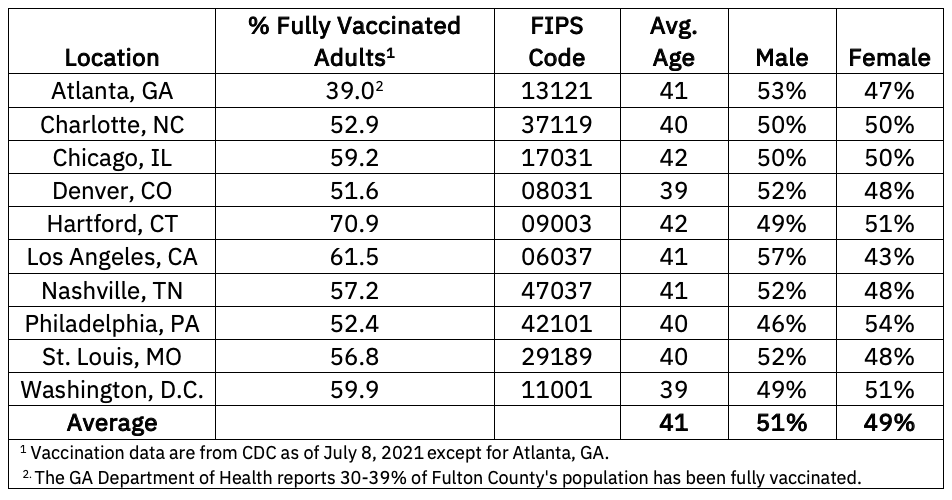
The simulations were run from June 1 through December 31, 2021 and accounted for protection afforded by previous COVID-19 infections and vaccination coverage in the counties where the cities are located. The study assumed that businesses would open their offices on August 16, 2021 and each of the cities would have lifted all mask requirements, social distancing, and capacity restrictions by the same date. The scenarios in which the workforce was not fully vaccinated also considered the impact of unvaccinated employees wearing or not wearing masks in the workplace.
Simulations modeled everyday behaviors of each company’s employees as well as those living in the same county and replicated their movement and exposures between their household, workplace, and neighborhood in combination with all the other people in the county. If an employee was infected at any point during the 4 months after businesses opened their offices, they were included in the study. The methodology used for the simulations accounts for the specific local demographics, travel, vaccine acceptance, population density, and vaccination coverage.
The three vaccination policy scenarios for each hypothetical company in each city were simulated multiple times and an average result was computed. The simulations evaluated the impact of mask wearing in the workplace for unvaccinated employees in the simulations that tested the policy that encouraged vaccination and no vaccination policies. Mask wearing was not included in scenarios where 100% of employees were vaccinated.
The estimated number of missed work-days and costs related to acute and recurrent (“long COVID”) symptoms from COVID-19 were computed and are presented below. For all cities included, the simulations produced no employees who became sick with COVID-19 if they were working at a company with a required vaccination policy; therefore, missed workdays and associated costs from acute and “long-COVID” were avoided. Simulated companies that strongly encouraged vaccination before entering the workplace fared better than companies with no vaccination policy—meaning they had 60% fewer missed workplace absences due to illness or exposure and 59% lower costs associated with COVID-19, on average.
Lost productivity and health costs associated with employee absences and long-term COVID-19 case management were evaluated. The study did not account for comorbidities within the employee population, but the assumption would be that the greater prevalence of comorbid conditions, the greater the long-term costs.
There is a clear winner among these strategies, but even if organizations do not want to take the stance that employees must be vaccinated before returning to the office, there would be fewer missed days of work and lower health costs if organizations strongly encourage their employees to get vaccinated rather than not having any policy at all. The study showed most infections occurred in households and neighborhoods rather than in the workplaces, but asymptomatic employees can bring that illness to the workplace and expose others. With few exceptions, companies in counties with lower vaccination rates had the greatest number of missed work days and higher costs if they did not have a vaccination policy compared with companies in counties with higher vaccination rates. In summary, organizations who require or strongly recommend getting vaccinated will more effectively reduce risks and costs associated with COVID-19.
“All companies, especially those in areas with low vaccination coverage, should consider adopting proactive vaccination policies to improve the safety and productivity of the workplace,” said Lisa Koonin, Founder of Health Preparedness Partners.
Employers do recognize that some employees may not receive a vaccination because of medical or religious reasons. Recently updated EEOC guidance emphasizes the employer’s role in providing accommodations for those employees as well as protecting employees that are vaccinated but immunocompromised.
Within the study, the policy that required 100% of employees at the workplace to be vaccinated did not show any infections occurring among the employee populations. If the study was expanded to run 100s of simulations for each scenario or included multiple businesses of 1,000 or more employees in each city, it might reveal the small probability that even with 100% of employees being vaccinated that an employee could get infected. This possibility may increase if the delta variant spreads further and erodes vaccine effectiveness.4
In addition to vaccinations, there is an array of protective measures organizations can deploy to ensure the health and safety of all employees, whether vaccinated or not. Polls have shown employee preferences for a hybrid working schedule which can also reduce exposures in the workplace.5 The Centers for Disease Control and Prevention (CDC) and several jurisdictions currently recommend that unvaccinated people wear a mask when in public settings.6 The study simulated the benefits of unvaccinated employees wearing masks in the workplace, and found on average, that mask wearing among unvaccinated employees would decrease infections in the workplace by more than 50%, prevent 65 missed days, and decrease the health costs by 9%. Mask wearing, social distancing, environmental cleaning, improving indoor air handling, self-screening, hybrid work models,7 and periodic testing are all well documented strategies to further decrease the risks to employee health that cause disruptions to business.8
“Overwhelmingly, we see that without a company-wide vaccination policy, firms could lose over a million dollars in COVID-19- associated health costs,” said John Cordier, CEO of Epistemix. “Encouraging employee vaccination can cut that number by about half.”
Contact us to learn more about this simulation or how to safely plan your return to the office and create a more resilient business.
Epistemix is a leading provider of analytical tools that empower leaders to make better decisions by simulating how diseases, ideas, and behavior spread through communities. We leverage decades of epidemiological experience, diverse datasets, realistic population dynamics, and scientific best-practice to build computational models that forecast the human impacts of policy interventions, so that organizations can take informed action. Our simulations have been used by groups like the Centers for Disease Control, the National Institutes of Health, and the World Health Organization. We are currently working with companies, event organizers, schools, and state and local governments across the United States to evaluate opening strategies and gauge COVID-19 response.
Health Preparedness Partners helps organizations respond to the COVID-19 pandemic by providing practical and detailed guidance about determining when and how to return to the workplace, strategies for protecting employees and managing ongoing risks, and preparing for future waves of COVID-19, as well as other threats. We bring decades of experience to help clients navigate complex pandemic response issues, having lead national and international efforts to combat Zika, Ebola, H1N1, and more. See HPP's guide to determining a workplace vaccination policy.
NOTES
Lost productivity attributed 10 missed days per infected individual as well as for the individuals who were in close contact with the infected individual while at work. Approximately, 15% of acute cases will require hospitalization which for self-insured employers may be on average $26,594 per individual. COVID-19 health costs for primary care, urgent care centers, and emergency departments settings were estimated from a data set of 2.5 billion claims that considered differences in cost by cities. The estimated health care costs of “long-haul” COVID-19 case management is not known, but one US study assumed 13% of all COVID-19 cases will lead to long-term symptoms and costs that can be as much as $100,000 per individual.9, 10, 11, 12
Other considerations in the model included variant strains, vaccine effectiveness for each strain, possible waning immunity after being infected or vaccinated, and for each employer policy there was an assumed level of vaccination coverage among the employees: 100% for required, 70% for encouraged, and 50% for no policy. The scenarios were simulated using the Epistemix FRED 7.0 software.
1More information about factors that influence the timing of return to workplace
3More information on these policies
5Pew Study on Changing Workforce Preferences
6CDC, 2021 and OSHA, 2021