Estimating Acute Asthma ER Visits Resulting from the Dixie Fire
The Dixie Fire in Greenville, CA has been raging since July 14, 2021, bringing destruction to those in its path. As of September 13, over 960,000 acres of land have burned, more than two times the California annual average. This is California’s second largest wildfire on record, the largest was the 2020 August Complex Fire, which burned just over 1 million acres. California usually accounts for around 80% of all Federal fires, and between 40-50% of all acres burned in the country annually. Reporting acres of land burned gives us a good estimate of the physical destruction affecting lives and livelihoods, but it doesn’t tell the full story on health impacts.
Wildfire smoke is a mix of gases and fine particles. It can make anyone sick, but is especially harmful for people at a greater risk of respiratory emergencies, such as those with asthma, COPD, or heart disease, as well as children, pregnant women and emergency responders. The Environmental Protection Agency’s Air Quality Index (AQI) is the measure widely used to report air quality. Higher values indicate greater levels of air pollution, and subsequently greater health risks. While members of sensitive groups mentioned above may be at higher health risk when the AQI measures above 100, everyone is in danger of being affected as the AQI climbs even higher. Usually charts show an upper limit of 500, mostly for convenience, but during wildfires the conditions can be off the charts. In the month of August in the area around the Dixie Fire, AQI peaked at 703 and was in the Hazardous range (above 300) for nine straight days in one county hit especially hard by the smoke.
Below, you can see asthma risk modeled across the affected population.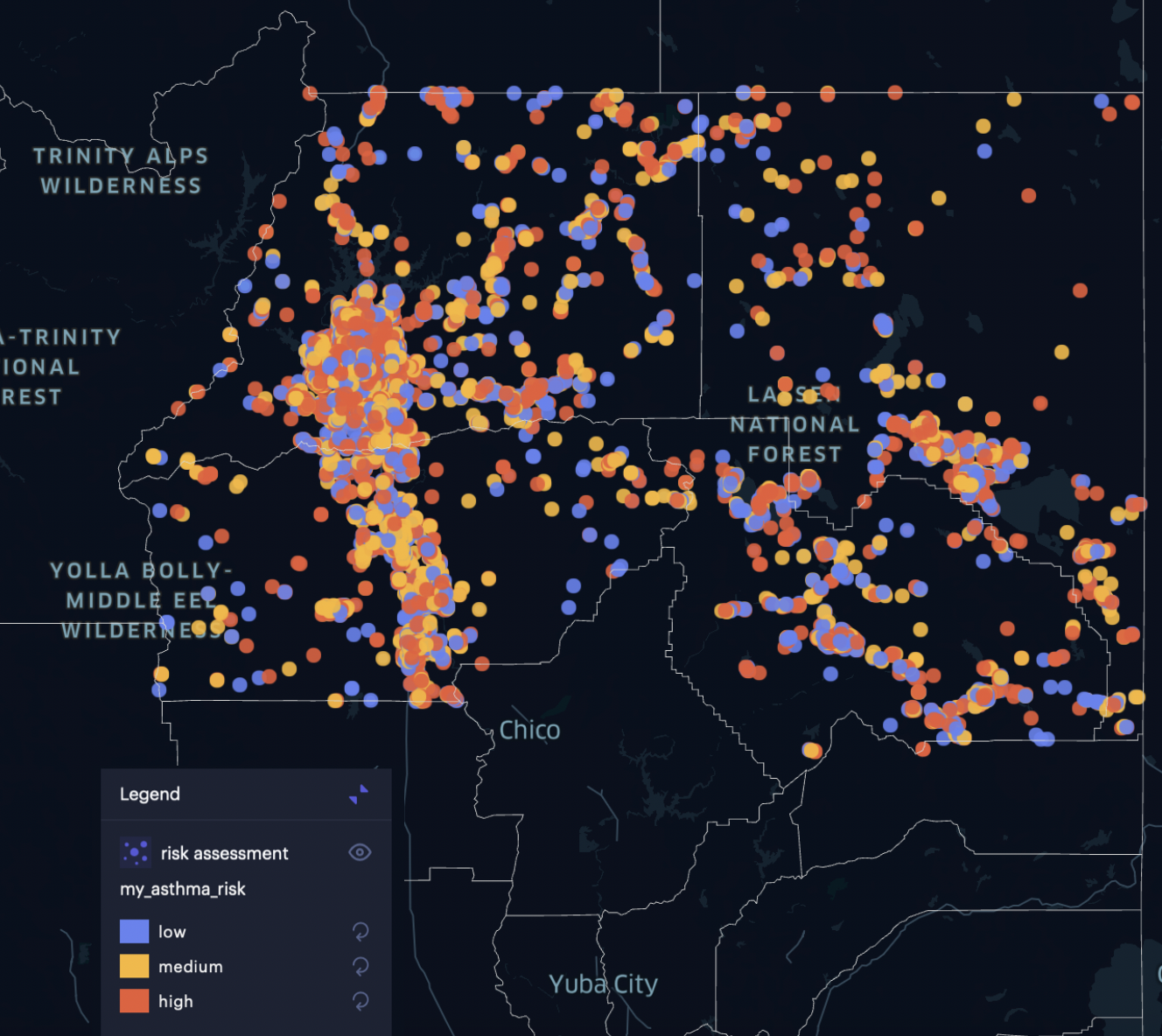 Wildfire smoke impacts human health in various ways. Acute asthma attacks skyrocket. Elevated AQI and increased particle pollution increase the risk of preterm birth (<37 weeks)—a 2021 study of births in California between 2006-2012 found that even one additional day of exposure to wildfire smoke during pregnancy can result in a measurable increase in preterm birth risk, and at “sample median smoke exposure (7 days) this translated to a 3.4% increase in risk, relative to an unexposed mother.” Increased risk of lung cancer and chronic asthma are other serious concerns.
Wildfire smoke impacts human health in various ways. Acute asthma attacks skyrocket. Elevated AQI and increased particle pollution increase the risk of preterm birth (<37 weeks)—a 2021 study of births in California between 2006-2012 found that even one additional day of exposure to wildfire smoke during pregnancy can result in a measurable increase in preterm birth risk, and at “sample median smoke exposure (7 days) this translated to a 3.4% increase in risk, relative to an unexposed mother.” Increased risk of lung cancer and chronic asthma are other serious concerns.
Health effects from wildfires range from acute illness to chronic conditions, each presenting its own challenges to local hospitals and health systems. At the most basic level, people living in the immediate vicinity of a wildfire might seek out urgent care due to burns, smoke inhalation, or other injuries resulting from being unable to evacuate quickly. At the same time, the surrounding counties may see greater hospitalizations due to the less tangible, but still very real threat of diminished air quality. Hospital systems already dealing with a baseline level of patients admitted to the ER on a daily basis suddenly have an influx of patients directly related to the wildfire as well as more patients admitted in response to respiratory distress. This can overwhelm even the most streamlined emergency department, and can lead to increased ER wait times, and even a shortage of beds or supplies.
Reading the headlines about the Dixie Fire, our team couldn’t help but wonder how the disaster was impacting local hospitals, and how many patients they should expect to serve if the fire continues unabated. If hospitals had access to that kind of data, maybe they could plan ahead and put the right staff and resources in place. So we decided to build a computational model that could figure it out.
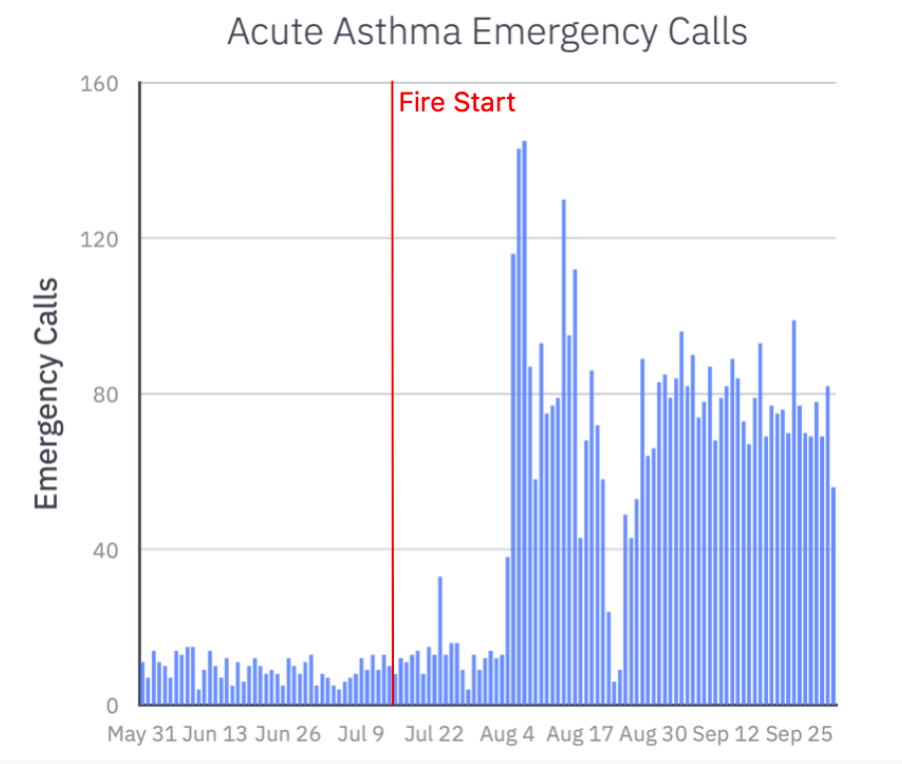
Because acute asthma attacks result in so many ER visits during wildfires, we focused our analysis on asthma risk. To model the health effects of the Dixie Fire, we added asthma risk as an attribute to our platform’s synthetic population based on demographics, and used daily county-level AQI data before and during the fire to simulate the impact of poor air quality on those at risk for acute asthma. Then we used personal asthma risk, elevation of household, and household location to estimate acute asthma cases resulting from elevated levels of poor air quality. These estimates are indicative of what realistic numbers could be, but would need to be integrated with real-world hospital visit data and asthma incidence data for the specific results to be actionable.
In the counties surrounding the Dixie Fire, the AQI value was above 150 for 26/30 days in August, creating sustained hazardous conditions for persons at risk. Normally, about 25% of people experiencing an acute asthma attack will need to be hospitalized. When air quality is at unhealthy levels for an extended period of time and people have nowhere to go to escape the cause of irritation, they often go to the ER for increasing shortness of breath, chest tightness, coughing and/or wheezing.
In our simulation, people suffering from acute asthma went to the hospital closest to their home, and there were an average of 59 daily hospital visits due to acute asthma during the fire to date, with variance according to local AQI values and population density.
So, what did the simulation reveal? If the fire continues at its current rate, we expect an additional 1,787 ER visits during the month of September in Plumas, Tehama, Shasta, and Lassen County hospitals due to acute asthma attacks, on top of regularly expected ER visits.
Data from the U.S. Department of Health and Human Services shows for the week of August 27 Shasta Regional Medical Center had 706 emergency department visits, and about 84% of its inpatient beds were filled. By taking our model results for September and calculating a weekly number per hospital, we project that about 55 of these visits were due to acute asthma symptoms related to the Dixie Fire, which amounts to about 20% of the real-world reported ER visits. It may be an even higher percentage, as the respiratory effects of diminished air quality would amplify the respiratory effects of the SARS-CoV-2 virus driving the ongoing Covid-19 pandemic.
Below, you can see how hospitals in densely populated areas with higher asthma risk are more likely to see higher ER visits.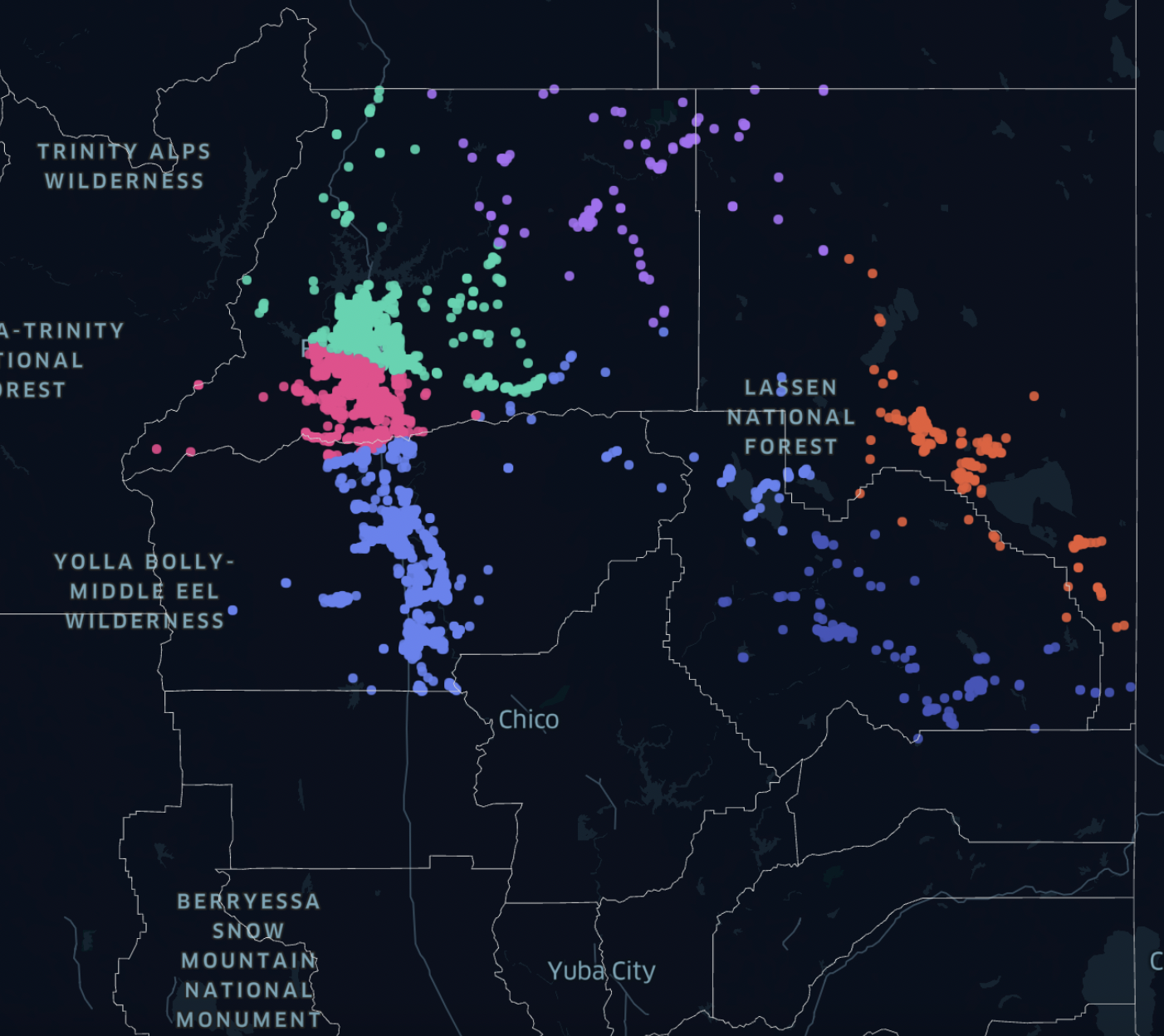 Estimating acute asthma cases and resulting emergency calls can help hospitals prepare for a health emergency by focusing resources where and when they are needed most.
Estimating acute asthma cases and resulting emergency calls can help hospitals prepare for a health emergency by focusing resources where and when they are needed most.
Hospitals can ensure they have extra respirators or asthma medication during wildfire season if they have an estimate of what the needs will be. Estimating increased ER wait times could facilitate an increase in hospital staffing during peak months, or alternatively, policies could be put in place to redirect patients to urgent care centers already primed for increased acute asthma patients to reduce strain on local emergency departments. With supplemental medical data or health insurance claims data, we could enhance our projections to include more detail and calibrate to real-world hospital visits.
As a society, we face unprecedented challenges with climate change, infrastructure failure, and a delicately balanced health system. Thankfully, we also have new tools to aid us in responding to these challenges. We can monitor for utility line breaks to catch and fix electrical infrastructure issues before they spark further problems. We have advanced medical knowledge of respiratory health, including preventative measures, pathways for disease, and treatment options. We can simulate demand for emergency care in an environmental health crisis so that healthcare providers can plan ahead and be prepared.
We all assume that the ER will be there for us in an emergency. But when a widespread disaster strikes, under-resourced ERs don’t have the time, people, or equipment to respond—leaving patients with nowhere to go for the help they so desperately need. It doesn’t have to be this way. Together, we can use the new tools at our disposal to build a more resilient health system, something we need now more than ever.
Cassie O’Connor is an intern at Epistemix.